Trigger Finger (Stenosing Tenosynovitis): Symptoms, Causes, Treatment, and Recovery
Introduction
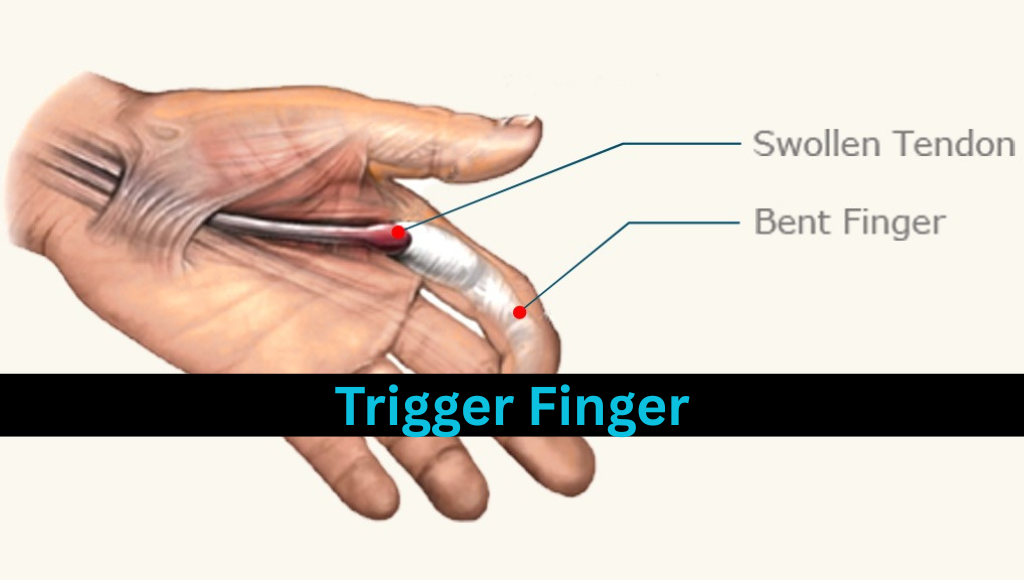
Trigger Finger, medically known as Stenosing Tenosynovitis, is a condition that affects the tendons in the fingers or thumb, leading to painful clicking or locking when the finger is moved. The condition can be mild or severe, and in some cases, the affected digit can become stuck in a bent position. It commonly affects people aged between 40 and 60 and is more prevalent among women and individuals with certain medical conditions such as diabetes or rheumatoid arthritis.
What is Trigger Finger (Stenosing Tenosynovitis)?
Trigger Finger is a condition that involves the tendons responsible for flexing the fingers and thumb. Each tendon in your fingers passes through a sheath lined with synovium—a slick membrane that allows the tendon to glide smoothly. In people with Trigger Finger, this sheath becomes inflamed or thickened, causing narrowing or the development of a nodule in the tendon, which inhibits smooth motion. The result is a “catching” or locking sensation when you try to straighten the finger.
Commonly Affected Fingers:
- Ring finger
- Middle finger
- Thumb (often called Trigger Thumb)
Causes and Risk Factors
While the exact cause of Trigger Finger isn’t always clear, several risk factors increase the likelihood of developing the condition:
1. Repetitive Hand Use
Tasks involving prolonged gripping or repeated finger movements can strain the tendons and lead to inflammation. This is common in:
- Manual laborers
- Musicians
- Farmers
- People who frequently use tools or keyboards
2. Medical Conditions
- Diabetes: People with diabetes are up to 10 times more likely to develop Trigger Finger.
- Rheumatoid Arthritis: Inflammation in the joints can also affect tendons.
- Gout and hypothyroidism may also increase susceptibility.
3. Gender and Age
- More common in women than men
- Usually affects individuals aged 40–60
Symptoms of Trigger Finger
The symptoms of Trigger Finger can vary in intensity and may develop gradually or suddenly:
1. Finger Stiffness
Especially noticeable in the morning, and may improve during the day.
2. Popping or Clicking Sensation
A snapping sound or feeling when moving the affected finger.
3. Tenderness at the Base of the Finger
Pain may be felt on the palm side of the hand near the base of the affected digit.
4. Finger Locking
In more severe cases, the finger may become locked in a bent position and require assistance to straighten.
5. Presence of a Lump
A small bump (nodule) at the base of the finger may be felt due to tendon swelling.
Diagnosis
Trigger Finger is usually diagnosed based on a physical examination. Your doctor may:
- Ask you to open and close your hand
- Feel for a nodule or clicking
- Observe locking behavior
No imaging is usually needed, although ultrasound or MRI can be used to rule out other tendon issues.
Stages of Trigger Finger
- Stage 1: Mild – Occasional clicking or pain; no locking
- Stage 2: Moderate – Frequent catching; finger may lock occasionally
- Stage 3: Severe – Persistent locking; finger may require manual straightening
- Stage 4: Fixed – Permanent bent position (requires surgical intervention)
Treatment Options
Treatment for Trigger Finger varies depending on the severity of the condition. The goal is to reduce inflammation, restore smooth tendon movement, and alleviate pain.
1. Conservative (Non-Surgical) Treatments
a. Rest and Activity Modification
Avoid activities that aggravate symptoms. Use of a splint may be recommended.
b. Splinting
Wearing a trigger finger splint or brace keeps the affected finger in a straight position, especially at night.
c. Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
Oral medications like ibuprofen help reduce pain and swelling.
d. Stretching and Exercises
Prescribed finger and hand exercises improve tendon flexibility and reduce stiffness.
e. Corticosteroid Injections
These injections reduce inflammation and are effective in many cases. However, repeated use may weaken the tendon.
2. Physiotherapy
Physical therapy plays a crucial role in non-surgical management:
- Ultrasound therapy
- Soft tissue mobilization
- Range of motion (ROM) exercises
- Strengthening exercises
3. Surgical Treatments
If conservative treatment fails or if the condition is advanced, surgery may be required.
a. Percutaneous Release
A needle is used to break the pulley that restricts tendon movement. Minimally invasive and performed under local anesthesia.
b. Open Surgery
An incision is made at the base of the finger to release the pulley. Recovery time is slightly longer but has a high success rate.
Post-Treatment Recovery
1. After Conservative Treatment
- Rest and hand therapy are critical
- Avoidance of aggravating activity
- Improvement can be seen within weeks
2. After Surgery
- Sutures are usually removed in 1–2 weeks
- Full recovery within 4–6 weeks
- Physical therapy may be recommended
Home Remedies and Lifestyle Tips
- Warm Compresses: Apply to reduce stiffness.
- Gentle Finger Massage: Increases blood flow.
- Finger Stretching Exercises: Improves mobility.
- Use Ergonomic Tools: Prevents strain during work.
Prevention
Though not all cases are preventable, the following steps can reduce your risk:
- Avoid prolonged gripping or repetitive hand use
- Use ergonomically designed tools
- Take regular breaks from typing or tool use
- Control underlying medical conditions like diabetes
Trigger Finger in Children
While rare, trigger thumb is the most common presentation in children, often visible at birth or during the first year. It typically doesn’t cause pain but may require surgical release if it does not resolve naturally.
Physiotherapy Treatment for Trigger Finger (Stenosing Tenosynovitis)
Physiotherapy plays a vital role in the conservative management of trigger finger. It focuses on reducing pain and inflammation, improving tendon gliding, restoring range of motion (ROM), and preventing recurrence. Below is a step-by-step breakdown of physiotherapy treatments:
1. Patient Education and Activity Modification
Goal: Prevent further tendon irritation.
What Physiotherapists Do:
Educate the patient about avoiding repetitive gripping or forceful finger motions.
Suggest ergonomic tools or aids (e.g., padded handles, ergonomic keyboards).
Recommend taking frequent breaks if the patient’s occupation involves repetitive hand use.
Advise against heavy lifting or prolonged vibration exposure (e.g., using power tools).
2. Splinting
Goal: Immobilize the affected finger to reduce inflammation and allow healing.
Types of Splints:
Static Splint: Keeps the finger in a neutral or slightly extended position (usually worn at night).
Dynamic Splint: Allows controlled motion to prevent stiffness while protecting the tendon sheath.
Usage:
Worn for 3–6 weeks, depending on severity.
Helps prevent triggering or locking of the finger during sleep and daily activities.
3. Cryotherapy (Cold Therapy)
Goal: Reduce acute inflammation and pain.
Application:
Use ice packs or cold compresses for 10–15 minutes at a time, several times a day.
Often applied before or after exercises to manage post-exercise soreness.
4. Thermotherapy (Heat Therapy)
Goal: Improve circulation and soften tissues for better mobility.
Application:
Warm packs applied for 15–20 minutes before therapy exercises.
Paraffin wax baths for the hand may also be used to increase tissue extensibility.
5. Ultrasound Therapy
Goal: Deep tissue heating and increased blood flow to aid healing.
Protocol:
Applied in pulsed or continuous mode over the affected tendon sheath area.
Duration: 5–8 minutes per session.
Frequency: 3 times per week in acute phase.
6. Soft Tissue Mobilization / Friction Massage
Goal: Break down adhesions and promote tendon mobility.
Technique:
Deep transverse friction massage (DTFM) directly over the thickened A1 pulley or tendon.
Duration: 5–10 minutes.
May be uncomfortable initially but effective in long-term relief.
7. Range of Motion (ROM) Exercises
Goal: Restore normal tendon glide and joint mobility.
Exercises:
Passive Finger Extension: Using the other hand to gently stretch the affected finger.
Active Tendon Gliding Exercises:
Hook fist
Straight fist
Full fist
Tabletop motion
Blocking Exercises:
Isolate movement of PIP and DIP joints to strengthen tendon coordination.
Frequency:
3–5 times daily, 10–15 repetitions each.
8. Strengthening Exercises (After Pain Reduction)
Goal: Improve grip strength and tendon resilience.
Tools:
Theraputty
Hand grippers
Resistance bands
Activities:
Squeezing putty or sponge
Pinching exercises
Rubber band finger abduction
⚠️ Caution: Start strengthening only after pain and locking reduce to avoid aggravation.
9. Taping and Kinesiology Taping
Goal: Reduce swelling and assist movement correction.
Application:
Taping along the tendon line and around the MCP joint.
Kinesiology tape may also be used to inhibit overactive muscles and support joint alignment.
10. Manual Therapy and Joint Mobilizations
Goal: Improve joint play and flexibility.
Techniques:
Grade I and II mobilizations for MCP and PIP joints.
Improve accessory movements to restore full ROM without pain.
11. Electrotherapy Modalities
Optional depending on severity
TENS (Transcutaneous Electrical Nerve Stimulation) for pain relief.
Interferential Therapy (IFT) to reduce deep-seated inflammation.
12. Postural and Ergonomic Advice
Goal: Prevent recurrence by correcting work or habit-related strain.
Examples:
Correct sitting posture during typing
Height and angle of tools or keyboards
Use of ergonomic mouse or pen
13. Home Exercise Program
A tailored set of exercises provided for daily practice to ensure consistent progress.
14. Progress Monitoring and Outcome Assessment
Physiotherapists assess progress every 1–2 weeks using:
Pain scales (VAS)
Finger locking frequency
ROM measurements
Functional hand use in ADLs (Activities of Daily Living)
Expected Outcomes of Physiotherapy
| Treatment Goal | Expected Timeline |
|---|---|
| Pain reduction | 1–2 weeks |
| Improved tendon gliding | 2–3 weeks |
| Elimination of clicking/locking | 3–4 weeks |
| Return to full function | 4–6 weeks |
✳️ In chronic cases, physiotherapy may be supplemented with corticosteroid injections or considered post-operatively for rehabilitation.
Other Related Article for reading
Frozen Shoulder Relief: Restore Movement and Comfort
What is trigger finger?
Trigger finger is a condition where a finger gets stuck in a bent position and may snap straight suddenly, like pulling a trigger.
2. Can trigger finger heal on its own?
Yes, mild cases may resolve without treatment, especially with rest and activity modification. Chronic or severe cases often need medical intervention.
3. What causes trigger finger?
It’s usually caused by repetitive hand use or gripping, leading to tendon inflammation in the fingers.
4. What office activities can cause trigger finger?
Activities like constant typing, clicking a mouse, or using tools that involve gripping can trigger the condition.
5. Can carpal tunnel syndrome lead to trigger finger?
Yes, carpal tunnel and trigger finger often occur together due to shared inflammation in the hand structures.
6. Does trigger finger cause arm, elbow, or shoulder pain?
While trigger finger mainly affects fingers, referred discomfort in the arm or shoulder can happen in severe or long-term cases.
7. Is trigger finger the same as Dupuytren’s contracture?
No. Trigger finger involves tendon inflammation, while Dupuytren’s contracture involves thickened connective tissue in the palm.
8. How is trigger finger diagnosed?
A doctor can usually diagnose it through physical examination and observing finger locking or clicking during movement.
9. What are the treatment options for trigger finger?
Treatments include rest, splinting, ice/heat therapy, NSAIDs, corticosteroid injections, or surgery.
10. Does heat help trigger finger?
Yes, heat can relax the muscles and tendons and increase blood flow to reduce stiffness.
11. Does ice help trigger finger?
Yes, icing the area can reduce inflammation and pain, especially after activity.
12. Can chiropractors treat trigger finger?
Some chiropractors use soft tissue techniques or ergonomic guidance to relieve tension, though it’s not a primary treatment.
13. Is acupuncture effective for trigger finger?
Acupuncture may help reduce pain and inflammation in some cases, though results vary between individuals.
14. Are trigger finger steroid injections painful?
There may be temporary discomfort, but the procedure is usually quick and well-tolerated.
15. How long does it take for steroid injections to work?
Improvements may be seen within a few days to a few weeks after the injection.
16. How long does trigger finger surgery take?
Surgery is usually a quick outpatient procedure, taking 15 to 30 minutes.
17. What kind of anesthesia is used for trigger finger surgery?
Local anesthesia is most commonly used; general anesthesia is rarely required.
18. Do compression gloves help trigger finger?
Yes, they may help reduce swelling and provide joint support.
19. How do you make a splint for trigger finger?
Use a padded aluminum splint or rigid tape to keep the finger extended, especially during sleep.
20. Is trigger finger considered a disability?
In severe cases affecting daily hand function, it may be considered a temporary disability and qualify for accommodations or medical leave.